News Letter, Vol. 4 (8), Auguse , 2012, © Copyright
Jun Xu, M.D. Lic. Acup., Hong Su, C.M.D., Lic. Acup.
Robert Blizzard III, DPT
Rehabilitation Medicine and Acupuncture Center
1171 East Putnam Avenue, Building 1, 2nd Floor
Greenwich, CT 06878
Tel: (203) 637-7720
Fax: (203)637-2693
Irritable Bowel Syndrome—IBS
Irritable Bowel Syndrome (IBS)
Lucy P. is a thirty-two-year-old student who came to me complaining of abdominal pain. She told me the pain is slow to come on. She feels it off and on and it can either be severe or mild. She also feels bloated and gaseous, and has constipation alternating with diarrhea, which produces mucus in the stool and is sometimes worse in the morning.
She generally feels mild depression, is shy and afraid to talk with people, and is unable to find a job. When she lived at home for five years after graduation, her parents encouraged her to go out and find employment, but her lack of communication skills made this impossible, so she decided to go back to school and earn a graduate degree in media communications. With graduation approaching, she began to feel nervous, knowing her parents expected her to get a job immediately after graduation. And she was depressed, experiencing insomnia, stomach aches, abdominal pain, and the bloating and diarrhea that sometimes turned to constipation. She was also vomiting and the pain and diarrhea she was experiencing interrupted her sleep and caused weight loss. She was frustrated with her condition, as were her parents, which is why she sought help from me.
A physical examination showed that Lucy had a soft abdomen, a normal bowel sound, no fever or chills, and a negative stool culture. I also sent her for a colonoscopy, which was negative as well. I determined that Lucy might have irritable bowel syndrome (IBS), a chronic gastrointestinal disorder of unknown cause, whose symptoms include the same abdominal cramping and pain, bloating, gassiness, and alternating bouts of diarrhea and constipation she was experiencing.
Unlike ulcerative colitis or Crohn’s disease, IBS is not an inflammatory intestinal disease. It does not cause inflammation or changes in bowel tissues, and it does not increase the risk of colorectal cancer. In many cases, IBS may be attributed to diet, lifestyle, and stress. It can be very difficult to diagnose because IBS is a diagnosis of exclusion. A CT scan and laparotomy study may be needed, even a colonoscopy, to first rule out cancer, gastritis, peptic ulcer, or the like. After all these diseases have been eliminated, it is then possible to make a diagnosis of IBS—irritable bowel syndrome.
Treatments in Western Medicine
People with irritable bowel syndrome should temporarily avoid all dairy products in order to rule out lactose intolerance, which sometimes mimics IBS. It is also necessary to avoid certain foods, such as the cruciferous vegetables—broccoli, Brussels sprouts, cabbage, and cauliflower—and beans as these can increase the bloating and gassiness. It may also help to increase the intake of fibers and try to decrease stress. If necessary, the doctor may prescribe antidepressant or antispasmodic medications, such as Bemote, Bentyl, and Lesin, or anti-diarrhea medication, such as Imodium. There are also some new medications that can probably help, such as tegaserod (brand name Zelnorm), used for the short-term treatment of IBS when constipation is the main symptom, and Lotronex, used for severe, chronic, diarrhea-predominant IBS. This latter drug may, however, cause many undesirable side effects, including death in men, so this treatment is approved only for women—and then, as for all pharmaceutical drugs, with caution.
Treatments in Traditional Chinese Medicine
The abdominal pain of this disorder is associated with the development of external disease and internal deficiency.Three types are associated with this condition.
- Type 1 is excessive coldness. Its main symptom is the abdominal pain, which becomes worse when the person drinks cold water. Also when the abdomen is exposed to cold in both the upper and lower extremities, that leads to low energy. In this case, the large intestine has no pushing force and and that triggers constipation; the person does not feel thirsty, however, and has long, cold urination. The principle of the treatment is to warm up the intestine and decrease the pain. The acupuncture points used are Ren 12 Zhong Wan, Ren 4 Guan Yuan, St 36 Zu San Li, and Sp 4 Gong Sun. The latter two can help decrease the coldness and improve the stomach movement, and St 36 and Sp 4 decrease the stomach ache and improve the spleen and stomach function.
Table 8-1
| Points | Meridian Number | Conditions Helped | |
| 1 | Zhong Wan | Ren 12
|
Stomach pain, abdominal distention, nausea, vomiting. GERD, diarrhea, dysentery,
|
| 2 | Guan Yuan | Ren 4
|
Enuresis, nocturnal emission, frequency of urination, diarrhea, abdominal pain, etc |
| 3 | Zu San Li | St 36
|
See Table 13.3 |
| 4 | Gong Sun | Sp 4
|
See Table 18.1 |
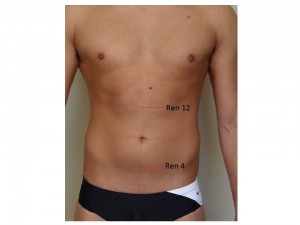
Please refer to the accompanying Figures (illustrations) for the
locations of the points. And please note that these illustrations are
for information only and may not show all the exact locations of
the acupuncture points.
Figure 8.1
Fig 8.2
- Type 2 is excessive hotness of the abdomen. This manifests itself in bloating, and in hardness and tenderness of the abdomen. The person craves cold water, becomes constipated, and experiences short, hot urination, and yellowish and dry coating of the tongue. The treatment for this condition is to eliminate the heat and treat the constipation. The acupuncture points are UB 25 Da Chang Shu, UB 24 Qi Hai Shu, St 37 Shang Ju Xu, LI 4 He Gu, LI 11 Qui Qi, St 44 Nei Ting, UB 24 and 25, and they are all very effective points to help bowel movements. LI 4 and LI 11 enhance the effectiveness of the rest of the points to improve bowel movements, so all these points together will increase pushing energy in the large intestine.
Figure 8.3
Table 8.2
| Points | Meridian Number | Conditions Helped | |
| 1 | Da Chang Shu | UB 25
|
Low back pain, diarrhea, constipation, muscular atrophy, pain, numbness and motor impairment of the lower extremities, sciatica |
| 2 | Qi Hai Shu | UB 24
|
Low back pain, irregular menstruation, asthma |
| 3 | Shang Ju Xu | St 37
|
Abdominal pain, diarrhea, dysentery, constipation, paralysis due to a stroke |
| 4 | He Gu | LI 4
|
See Table 12.1 |
| 5 | Qu Qi | LI 11
|
See Table 12.2 |
| 6 | Nei Ting | St 44
|
See Table 18.1 |
Please refer to the accompanying Figures (illustrations) for the
locations of the points. And please note that these illustrations are
for information only and may not show all the exact locations of
the acupuncture points.
- Type 3 is excessive activity of the liver qi (energy) causing abdominal pain. The main symptoms are abdominal pain, anxiety, depression, and panic attacks, as well as a pain that radiates to the chest, and shooting pains down the side of the abdomen that feel better after a deep sigh. The pain becomes worse during a panic attack, depression, or periods of anxiety. The principal treatment for this type of IBS is to regulate the liver energy and decrease the abdominal pain, so the acupuncture points used for treatment are Liver UB 18 Gan Shu, Liver 3 Tai Cong, and Liver 14 Qi Meng. Since these points all are related to the liver, they will calm the hyperactivity of the liver energy, and improve the liver’s function of regulating the stomach and the large intestine’s movement and function. St 25 Tian Shu and St 36 Zu San Li are the important points that help make the necessary adjustment to the stomach and large intestine and decrease the diarrhea and constipation. GB 34 Yang Ling Quan and RN 6 Qi Hai improve the energy flow of the abdomen and decrease muscle spasms in the bowels and stomach. Taken together, all these points will help for this type of IBS.
Table 8.3
| Points | Meridian Number | Conditions Helped | |
| 1 | Gan Shu | UB 18
|
Backache, blurred vision, epilepsy, jaundice, mental disorders, night blindness, redness of the eye, spitting blood |
| 2 | Tai Cong | Li 3
|
See Table 18.1 |
| 3 | Qi Men | Li 14
|
Acid regurgitation, depression, hiccups |
| 4 | Tian Shu | St 25
|
Abdominal pain, constipation, diarrhea, dysentery, irregular menstruation, swelling |
| 5 | Yang Ling Quan | GB 34
|
Bitter taste in the mouth, infantile convulsions, jaundice, numbness and pain of the lower extremities, swelling and pain of the knee, weakness, vomiting |
| 6 | Zu San Li | St 36
|
See Table 13.3 |
| 7 | Qi Hai | RN 6
|
Abdominal pain, nocturnal emission, impotence, hernia, swelling, diarrhea, dysentery, uterine bleeding, irregular menstruation, post-partum hemorrhage, constipation, asthma |
Please refer to the accompanying Figures (illustrations) for the
locations of the points. And please note that these illustrations are
for information only and may not show all the exact locations of
the acupuncture points.
Figure 8.4
Lucy’s Treatment
Lucy underwent treatment three times a week for five weeks, which greatly diminished her symptoms and gave her relief. I also prescribed some Chinese herbs for her constipation, and treated her depression with points on the top of her head (Shi Sheng Chong), which helped lessen her depression. Treating emotional disturbances is very important as it is one of the most effective remedies for IBS. Once Lucy’s depression, anxiety, and panic attacks were brought under control, her IBS symptoms were greatly reduced.
Tips for Personal Use
- Take it easy. Emotional stress is very harmful for IBS.
- Focus on acupressure points St 36 and RN 6. Acupressure the points with your thumb or knuckle, pressing with comfortable pressure on the points; count to 20, then change to another point.
- Get deep massages and use a heating pad.