News Letter, Vol. 5 (1), January , 2013, © Copyright
Jun Xu, M.D. Lic. Acup., Hong Su, C.M.D., Lic. Acup.
Robert Blizzard III, DPT
Rehabilitation Medicine and Acupuncture Center
1171 East Putnam Avenue, Building 1, 2nd Floor
Greenwich, CT 06878
Tel: (203) 637-7720
Fax: (203)637-2693
Post-Treatment Lyme Disease Syndrome
My dear friends,
Before you read my case discussion, please read the following ,
I was the president of American Traditional Chinese Medicine Society (www. http://atcms.org) between March 2010 and March, 2012. Now, I am honorary president of ATCMS. On behalf of ATCMS, I advise you sign the petition to urge Obama Administration recognize acupuncturist as healthcare providers and allow Medicare to pay acupuncture treatment.
Thank you for your support! Please sign the petition now!
Jun Xu, MD
Recognize Acupuncturist as Healthcare providers
Despite overwhelming evidence of the positive impact acupuncturist have on patient health, they are not recognized as healthcare providers under the Social Security Act and, therefore, cannot be paid by Medicare for therapy management.
Please visit the website at: https://petitions.whitehouse.gov/petition/recognize-acupuncturist-healthcare-providers/NTNpVFnp, and sign this petition to urge President to recognize acupuncturists as Medicare providers. We do need at least 25000 signatures by February 10, 2013, in order to get a response from the White House. Please forward this email to your family members, friends, and patients, and ask them to do so. Your participation will make a difference.
Thanks for your efforts and participating!
American TCM Society (ATCMS)
Fig 1-1
Janet, a 36 year old woman, came to me with complaints of body aches and multiple joint pain for the past 6 months. Janet reported, “Every inch of my body is achy, I am depressed.” She reports having a tick bite about ten months ago, while she was playing with her son in the backyard of her house. A dead tick was found on her neck close to her hair line with a bull’s eye rash prompting her to see her physician immediately and receiving antibiotics (doxycycline) for three weeks. She felt fine at that time. However, after one month, she started to develop some flu like symptoms; feeling fatigue, poor sleep, stomach cramps and poor appetite. She took advil for 2 weeks without any improvement. She also felt poor concentration along with severe headaches. Later she developed bilateral knee joint swelling, difficulty walking, a tingling like snake sensation at both legs and hands. She went to many different doctors for her symptoms, though no one could give her a definite answer and treatment, therefore, she came to me for help.
Janet is most likely to have Post-Treatment Lyme Disease Syndrome
Approximately 10 to 20% of patients treated for Lyme disease with a recommended 2–4 week course of antibiotics will have lingering symptoms of fatigue, pain, or joint and muscle aches. In some cases, these can last for more than 6 months. Sometimes it is called “chronic Lyme disease,” this condition is properly known as “Post-treatment Lyme Disease Syndrome” (PTLDS).
The main symptoms of PTLDS are listed as following,
- Arthritis. After several weeks of being infected with Lyme disease, approximately 60% of those people not treated with antibiotics develop recurrent attacks of painful and swollen joints that last anywhere from a few days to a few months. The arthritis can shift from one joint to another; the knee is most commonly affected and usually one or a few joints are affected at any given time. About 10% to 20% of treated patients will go on to develop lasting arthritis. The knuckle joints of the hands are only very rarely affected.
- Neurological symptoms. Lyme disease can also affect the nervous system, causing symptoms such as stiff neck and severe headache (meningitis), temporary paralysis of facial muscles (Bell’s palsy), numbness, pain or weakness in the limbs, or poor coordination. More subtle changes such as memory loss, difficulty with concentration, and a change in mood or sleeping habits have also been associated with Lyme disease. People with these latter symptoms alone usually don’t have Lyme disease as their cause.
Nervous system abnormalities usually develop several weeks, months, or even years following an untreated infection. These symptoms often last for weeks or months and may recur. These features of Lyme disease usually start to resolve even before antibiotics are started. Patients with neurologic disease usually have a total return to normal function.
- Heart problems. Fewer than one out of 10 Lyme disease patients develops heart problems, such as an irregular, slow heartbeat, which can be signaled by dizziness or shortness of breath. These symptoms rarely last more than a few days or weeks. Such heart abnormalities generally appear several weeks after infection, and usually begin to resolve even before treatment.
- Other symptoms. Less commonly, Lyme disease can result in eye inflammation and severe fatigue, although none of these problems is likely to appear without other Lyme disease symptoms being present.
The exact cause of PTLDS is not yet known. Most medical experts believe that the lingering symptoms are the result of residual damage to tissues and the immune system that occurred during the infection. Similar complications and “auto–immune” responses are known to occur following other infections, including Campylobacter (Guillain-Barre syndrome), Chlamydia (Reiter’s syndrome), and Strep throat (rheumatic heart disease). In contrast, some health care providers tell patients that these symptoms reflect persistent infection with Borrelia burgdorferi. Recent animal studies have given rise to questions that require further research, and clinical studies to determine the cause of PTLDS in humans are ongoing.
Regardless of the cause of PTLDS, studies have not shown that patients who received prolonged courses of antibiotics do better in the long run than patients treated with placebo. Furthermore, long-term antibiotic treatment for Lyme disease has been associated with serious complications. The good news is that patients with PTLDS almost always get better with time; the bad news is that it can take months to feel completely well.
If you have been treated for Lyme disease and still feel unwell, see your doctor to discuss how to relieve your suffering. Your doctor may want to treat you in ways similar to patients who have fibromyalgia or chronic fatigue syndrome. This does not mean that your doctor is dismissing your pain or saying that you have these conditions. It simply means that the doctor is trying to help you cope with your symptoms using the best tools available.
It is normal to feel overwhelmed by your ongoing symptoms. Some things that may help you manage your PTLDS include:
- Check with your doctor to make sure that Lyme disease is not the only thing affecting your health.
- Become well-informed. There is a lot of inaccurate information available, especially on the internet. Learn how to sort through this maze.
- Track your symptoms. It can be helpful to keep a diary of your symptoms, sleep patterns, diet, and exercise to see how these influence your well being.
- Maintain a healthy diet and get plenty of rest.
- Share your feelings. If your family and friends can’t provide the support you need, talk with a counselor who can help you find ways of managing your life during this difficult time. As with any illness, Lyme disease can affect you and your loved ones. It doesn’t mean that your symptoms are not real. It means that you are a human being who needs extra support in a time of need.
- Being strong mind, if you know the mechanism of your illness and have strong mind to fight this illness, you will finally get out of the control of the disease.
It is important to note that people with a history of Lyme disease have more musculoskeletal impairments when compared to those without a history of the disease. Physical Therapy is very effective at treating musculoskeletal impairments such as pain and muscle spasms though multiple means of massage, heat, ultrasound, electrical stimulation. Muscle weakness and limited endurance are other symptoms that can be greatly improved with treatment.
A common impairment is decreased standing balance and impaired gait pattern that a routine of lower body strengthening, core training and balance exercises would help to restore. Functional limitations would include difficulty with stair negotiation; sit to stand transfers and the inability to continue to work. It is important not to over stress yourself with exercise or daily activities to prevent from exacerbating your PTLDS
A few exercises would be a light general warm-up that is easy on the knees being the exercise bike at low-moderate intensity taking breaks as needed.
Fig 1-2 http://visionfitness.mercola.com/exercise-bikes.aspx
After warmed-up, a whole body exercise that also works on a common ailment of decreased transfer ability with sit to stands would be chair squats. With this exercise it is important not to allow your knees to track beyond your toes and to barely allow the hips to touch the seat before standing back up again. Start with 10 pain free reps and working up to 30 reps total.
Fig 1-3 http://holistichealthgurus.com/blog/body/squats-with-chair-facing-the-wall/
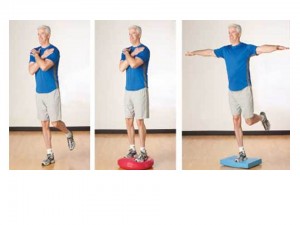
Balance is another ailment that can be worked with exercise. Start out on a flat surface with eyes open for one minute, once that becomes easy start to challenge yourself by closing your eyes only as long as you are standing in front of a couch or table that you can grab hold of if needed. Continue to progress by then standing on a foam pad to make the surface uneven or stay on the flat surface and stand on one foot at a time with eyes open and then closed.
Fig 1-4 http://www.acefitness.org/certifiednewsarticle/687/designing-balance-exercise-programs-for-older/
A light stretching routine is encouraged to decrease joint stiffness and improve range of motion. Shown is a simple stretch that if held for 1 minute on each leg will loosen muscles around the most common effected area with PTLDS being the knees.
Fib 1-5 http://www.livestrong.com/slideshow/558801-finding-the-fitness-30/#slide-2
Acupuncture is an excellent alternative way to treat your symptoms. It has no side effects and can be combined with traditional western medicine to relieve your symptoms. The choice of acupuncture treatment of PTLDS is as following,
- Common used points: Du20 Bai Hui, GB8 Shuai Gu, UB9 Yu Zhen, Ht7 Shen Men, GB20 Feng Chi, UB15 Xin Shu, UB20 Pi Shu, UB18 Gan Shu, UB23 Shen Shu, St6 Zu San Li, Sp6 San Yin Jiao, Lv3 Tai Cong, UB2 Zan Zhu, Kid3 Tia Xi.
- Arthritis: Shoulder: LI 15 Jian Yu, SI 9 Jian Zhen, SJ 14 Jian Liao, SI 10 Nao Shu, SI 11 Tian Zhong, LI 16 Ju Gu Wrist: LI5 Yang Xi and SJ 4 Yang Chi. Knee: LI 4 He Gu, LI 11 Quchi, St 35 Du Bi, Nei Xi Yan, Sp 10 Xue Hai, St 34 Liang Qiu, He Ding, UB 40 Wei Zhong, ,
- Neurological Symptoms: Fatigue, Depression and Poor Sleep: Major points: St 36 Zu San Li, PC6 Nei Guan, LI4 He Gu, Ht7 Shen Meng, Sp6 San Yin Jiao, GB20 Feng Chi, Du20 Bai Hui, EX-HN1 Si Shen Cong, assistant points: Du14 Da zhui, Ren12 Zhong Wan, Ren14 Ju Que, Ren6 Qi Hai, Ren4 Guang Yuan, UB21 Wei Shu and UB23 Shen Shu.
- Bell’s Palsy: GB14 Yang Bai penetrating Ex Yu Yao, and Si Bai, Tai Yang penetrating St7 Xia Guan, St4 Di Chang penetrating St6 Jia Che, LI20 Ying Xiang, UB2 Zan Zhu, Ren24 Cheng Jiang.
- Heart Palpitation: PC6 Nei Guan, Ht7 Shen Men, UB15 Xin Shu, Ren14 Ju Que, UB14 Jue Yin Shu
- Dizziness: Si Shen Chong, Du20 Bai Hui, Du12 Shen Zhu, UB12 Feng Men, UB43 Gao Huang, Sp6 San Yin Jiao, St36 Zhu San Li, LI11 Qu Chi.
Janet’s Treatment:
Janet was treated with me for 2 x per week for 8 weeks. I first try to decrease her pain at the joints and body with the points of group 1 and 2 , then, I used the group 3 points to help her to improve her fatigue and depression, after about 2 month’s treatment, Janet felt much improved. Her pain scale decreased from 9/10 to 2/10. She then had maintenance treatment for once a week for another 2 weeks, she finally discharged without pain.
Tips for Patients:
- Early diagnosis and early treatment: Always suspect you might have Lyme disease if you have exposed to wild environment with skin rash. Early treatment is the key to reduce the rate of Post Treatment of Lyme Disease Syndrome.
- Multiple Therapy is the best way to treat PTLDS. Anti-inflammatory Medication, Physical Therapy and Acupuncture Treatment together will help you a lot.
Tips for Acupuncturists:
- Treat your patients as a whole person, you not only treat their pain symptom, but also their stress, fatigue, and depression. To relieve the mental stress is the key for the effects of your acupuncture treatment.
- Encourage your patients to have at least 8 weeks treatment. It is very important to have a long term treatment to achieve the best results.
References
Reviews of human research
Marques, A. Chronic Lyme disease: a review. Infect Dis Clin North Am 2008; 22:341–60.
Feder, et al. A critical appraisal of “chronic Lyme disease”. New Eng. J. Med. 2008; 357:1422–30.
Non-human research
The following publications refer to studies in mice and monkeys. Please note that while animal studies are helpful, further research is necessary to determine whether these results correlate with human disease.
Barbour A. Remains of infection. J Clin Invest. 2012 Jul 2;122(7):2344–6. doi: 10.1172/JCI63975. Epub 2012 Jun 25.
Bockenstedt LK, Gonzalez DG, Haberman AM, Belperron AA. Spirochete antigens persist near cartilage after murine Lyme borreliosis therapy. J Clin Invest. 2012 Jul 2;122(7):2652–60. doi: 10.1172/JCI58813. Epub 2012 Jun 25.
Embers ME, Barthold SW, Borda JT, Bowers L, Doyle L, et al. (2012) Persistence of Borrelia burgdorferi in Rhesus macaques following antibiotic treatment of disseminated infection. PLoS ONE 7(1): e29914.
Reference resource:
http://www.webmd.com/rheumatoid-arthritis/arthritis-lyme-disease
http://www.cdc.gov/lyme/postLDS/index.html