News Letter, Vol. 1 (4), April, 2009, © Copyright
Jun Xu, M.D. Lic. Acup., Hong Su, C.M.D., Lic. Acup.
www.rmac.yourmd.com
www.drxuacupuncture.co
Rehabilitation
Medicine and Acupuncture Center
1171 East
Putnam Avenue, Building 1, 2nd Floor
Greenwich, CT 06878
Tel: (203) 637-7720
Case Discussion 4 – Osteoporosis
Patient Name: Emily M.
Emily M. is 59 years old female.
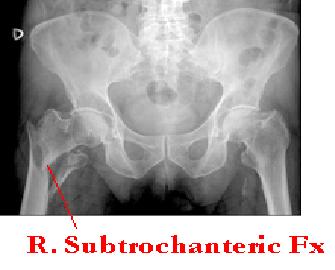
About one week ago, when she opened her garage and tried to take her garbage can out of her house, she had a fall and she immediately felt severe pain in the right hip and she had difficulty to getting up from the ground. Her husband immediately called 911 and Emily was taken to the hospital. In the ER an x-ray was done which showed a fracture (Fx) of the right hip. The patient had an immediate operation for a total hip replacement because she had severe osteoporosis and her bone age is more than -2.5 SD as shown by a bone scan. After the operation, she came to my office for rehabilitation, and she asked me why it is so easy to have a fracture. Her friends sometimes had falls without any problems. She wanted acupuncture treatments and also a nutritional consultation about her osteoporosis.
I asked her past medical history. When she was young Emily was an athlete. She ran about five miles a day five days a week for about 10 years, so she was very thin and skinny during this period. When she was between 16 and 26 she rarely menstruated. After she stopped her marathon training she gradually recovered her menstruation. Then, she got pregnant. She has two children and she told me her mother also had a fall at age 55 and also had a Lumbar 4 and 5 veterbrate compression fracture. She asked me if there was any connection between her mom’s fall and her own.
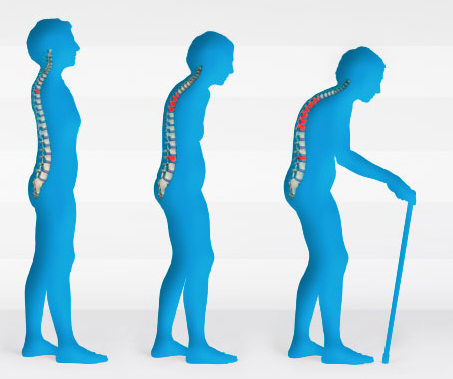
Emily has osteoporosis, which is often seen in women of postmenopausal age and men above age of 75. Osteoporosis usually does not show any symptoms until one day a fracture occurs. Women and men with osteoporosis most often break bones in the hip, spine, and wrist. The fracture of the bone in an old person could be a warning sign that the bone is weaker than optimal. A fracture of the long bone such as hip and wrist are acute impaired mobility, and they require surgery. The symptoms of vertebral collapse, usually exhibit sudden back pain often with radicular pain shooting down to the legs with numbness and tingling sensation. This fracture usually is called a compression fracture and by x-ray, you can see the vertebral collapse. If there are multiple vertebral fractures (Fx), you will see the patient has a stooped posture, loss of height, and chronic pain with reduction of mobility.

Risk Factors For Osteoporosis:
All post menopausal women and men age 50 and older should be evaluated clinically for osteoporosis risk factors in order to determine the need for bone mineral density testing. Osteoporosis is preventable if we identify the risk factors for the patients and therefore a fall causing the fracture of a bone can be avoid.
The most identifiable risk factors are as following:
1.
Genetic factors: There are many genetic factors that will cause osteoporosis such as parental history of hip fracture, cystic fibrosis, hypophosphatasia, idiopathic hypercalcinuria, etc.
2.
Lifestyle factors such as low calcium intake, vitamin D insufficiency, excessive vitamin A intake, high caffeine intake, high salt intake, alcohol: three or more drinks a day, immobilization, inadequate physical activity, smoking, tennis, and excessive physical activity. There are numerous examples of marathon runners who develop severe osteoporosis late in life. In women, heavy exercise can lead to decreased estrogen levels, which inhibit the calcium absorption and produce osteoporosis. In addition, intensive training without proper calcium and vitamin D and nutrition compensation will increases the risk of osteoporosis and fracture. Soft drinks, which contains phosphoric acid may increase the risk of osteoporosis because the phosphoric acid will displace calcium contained in the bone.
3.
Medications: Many medications are associated with osteoporosis and fracture.
1). Glucocorticoids i.e. steroid. If you take more than 5 mg per day of prednisone or equivalent for more than three months, usually it will cause osteoporosis.
2). Anticoagulants such as heparin.
3). Chemotherapeutic drugs.
4). Anticonvulsant.
5). Barbiturate.
6). Cyclosporin A, tacrolimus, lithium, etc.
4.
Diseases and disorders. There are many diseases associated with osteoporosis:
1). Endocrine disorders such as Cushing’s syndrome, hyperparathyroidism, thyrotoxicosis, diabetes mellitus, adrenal insufficiency, etc.
2). Malnutrition, parenteral nutrition, and malabsorption such as Crohn’s disease, ulcerative colitis, lactose intolerance, gastrectomy surgery, intestinal bypass surgery or bowel resection, vitamin K and vitamin B12 deficiency, etc.
3). Renal insufficiency.
4).
Hematological disorders such as multiple myeloma, leukemia, lymphoma, sickle cell disease, etc.
5).
Hypogonadal disease such as Turner syndrome, Klinefelter syndrome, Kallmann syndrome, anorexia nervosa, etc.
Who gets osteoporosis?
Osteoporosis is more common in elder individuals and Caucasian woman, but osteoporosis can occur at any age in men as well as in women and in all ethnic groups.
About 10 million Americans have osteoporosis, 80% of them are women. One in two women has a fracture related to osteoporosis in her lifetime. Thus, women over the age of 50 are at greatest risk of developing osteoporosis and suffering related fractures.
Osteoporosis can begin at a young age if a person does not get enough calcium and vitamin D. After reaching maximum bone density and strength between the ages of 25 and 30, a person loses about 0.4% of bone strength each year. At this rate and with good nutrition, people should experience bone loss without developing osteoporosis.
However, after menopause, women lose bone mass at a higher rate as high as 3% per year. After menopause, a women’s body makes much less estrogen. Estrogen is a hormone substance that flows in the blood to control body functions. It helps to prevent osteoporosis. In fact, osteoporosis is secondary to the body that cannot make enough new bone and to compensate the body’s loss of the old bone.
How to diagnose osteoporosis?
The dual-energy absorptiometry DXA measures the hip and the spine bone density to establish or confirm the diagnosis of osteoporosis, predict future fracture risk, and to monitor patients by performing serial assessments. WHO, the World Health Organization has established the following definition based on BMD (Bone Mineral Density) measurements at spine, hip, or forearm by DXA devices.
Normal BMD is within 1 SD of a young normal adult, T-score at 1.0 and above.
Low bone mass osteopenia, BMD is between 1.0 and 2.5 SD (Standard Deviation) below that of a young normal adult, i.e. T-score between -1.0 and –2.5.
Osteoporosis, BMD is 2.5 SD or more below that of a young normal adult, T-score at or below –2.5. Patients in this group who have already experienced one or more fractures are deemed to have severe or established osteoporosis.
Who should be tested for BMD?
Based on National Osteoporosis Foundation conditions’ guide, the following people should be tested for BMD.
1. In women age 65 and older and men age 70 and older, recommend BMD test.
2. In postmenopausal women and the men age 50 to 69 recommend BMD testing when the doctor has concerns based on their risk factor profile.
3.
Recommend BMD testing to those who have had a fracture to determine degree of disease’s severity.
How is osteoporosis treated?
1. The most important treatment is prevention.
1).
Calcium 1000 mg per day should be taken for women before menopause and a 1200 mg per day for women who are postmenopausal.
2).
Vitamin D 800 IU for women before menopause and 1000 IU vitamin D for postmenopausal women. Men up to age of 50 should increase vitamin D and calcium intake to 800 IU of vitamin D and 1000 mg of calcium per day.
There are numerous calcium products in the market. Most of them are in tablet form, which is difficult for your body to absorb, because the calcium supplement is not blended with vitamin D and magnesium; these are necessary to aid in the absorption and use of calcium.
Even if the calcium tablet is blended correctly, it may be difficult for the body to utilize or break down the calcium. One explanation may be that many calcium brands use calcium from eggshell or oyster shell. These may not be well absorbed by the body. Another reason calcium may not be absorbed from a tablet is because of DCP, which is a binding agent used to hold the tablet together. DCP does not break down in the body.
In addition to binders, some calcium supplements may have additives such as chlorine and other chemicals. Even assuming no binders are used in the calcium tablet, the body must still break down a hard-pressed tablet into a usable form. If the tablet cannot be broken down sufficiently in the stomach, then the calcium will not be absorbed. If you can’t break down the calcium your body is robbed of the calcium needed to support bodily functions.
Based on the above analysis, I strongly urge you not take the tablet form of calcium. After careful study, I believe that Nutrametrix supplies the best calcium, i.e. blended with Vitamin D3 and magnisium, isotonic form.
2. Regular weightbearing exercise. Increased walking, jogging, tai chi, stair climbing, dancing, and tennis. Muscle strengthening exercises include weight training and other resistive exercise. Weightbearing exercise programs not only increase bone density but also improve both heart and lung functional ability and muscle strength.
3. For prevention, you should take all preventative procedures such as checking and correcting vision and hearing, evaluating any neurological problems, reviewing any prescription medications for side effects that may affect balance, and providing a check list for improving safety at home. Wearing undergarments with hip pad protectors may protect an individual from injuring the hip in the event of a fall. Hip protectors may be considered for patients who have significant risk factors for falling or for patients who have a previously fractured hip.
4. Avoidance of tobacco use and excessive alcohol intake. Alcohol and cigarettes inhibit osteoblast cell activities and improve osteoclast cell functioning. Osteoclast cells usually destroy the bone density and osteoblast cell build up the bone density.
Medical treatment for osteoporosis:
1. For the patient who has vertebral or hip fracture.
2. DXA hip or spine T-score is less or equivalent to –2.5.
3. Low bone mass and US adopted WHO 10-year probability of hip fractures more or equivalent to 3% or 10 years probability of any major osteoporosis related fractures more than 20%.
The following are the FDA approved medications for treatment of osteoporosis:
1. Bisphosphonates.
a.
Alendronate, brand name, Fosamax. Alendronate reduces the incidence of spine and hip fractures by about 50% over three years in patients with prior vertebral fracture. It reduces the incidence of vertebral fractures by about 48% over three years in patients without prior vertebral fracture.
b.
Ibandronate, brand name, Boniva. Boniva reduces the incidence of vertebral fractures by about 50% over three years.
c.
Risedronate, brand name, Actonel with calcium. Risedronate reduces the incidence of vertebral fractures by about 41& to 49% and the nonvertebral fractures by about 36% over three years with significant risk reduction occurring after one year of treatment in patients with a prior vertebral fracture.
d.
Zoledronic acid, brand name, Reclast. Zoledronic acid is approved by FDA 5 mg/IV infusion over at least 50 minutes once yearly for osteoporosis in postmenopausal women. Reclast reduces the incidence of vertebral fractures by about 70% with significant reduction at one year, hip fractures by about 41%, and nonvertebral fractures by about 25% over three years.
There are many side effects for bisphosphonates, such as GI problems, difficulty swallowing, inflammation of esophagus, and gastric ulcer. All these medications must be taken on an empty stomach first thing in the morning with at least 8 ounces of plain water.
There are also other treatments for osteoporosis.
1. Calcitonin: the brand name is Miacalcin or Fortical. Oral salmon calcitonin is FDA approved.
2. Estrogen hormone therapy. For estrogen hormone therapy, the Women’s Health Initiative reported increased risks of myocardial infarctions, stroke, invasive breast cancer, pulmonary emboli, and deep vein phlebitis during five years of treatment with conjugated equine estrogen and medroxyprogesterone, however, subsequent analysis of those data showed no increase in cardiovascular disease, therefore, the use of the estrogen hormone treatment is recommended for only shortest duration and the lowest effective doses. All the clinicians must evaluate the risks before considering giving patient this hormonal treatment.
3. Parathyroid hormone PTH, brand name, Forteo, is approved by FDA for treatment of osteoporosis in postmenopausal women at high risk for fracture, however, there is increased incidence of osteosarcoma in rats. The usage of parathyroid hormone is cautious.
How acupuncture helps osteoporosis:
Traditional Chinese Medicine thinks osteoporosis mainly is caused by kidney deficiency, therefore, the most important thingin TCM is to protect kidney function and acupuncture usually cannot treat the fractured bone, however, acupuncture can help by improving and
adjusting the stomach and large intestine natural absorption for calcium, phosphate, magnesium, etc., to prevent mineral loss.
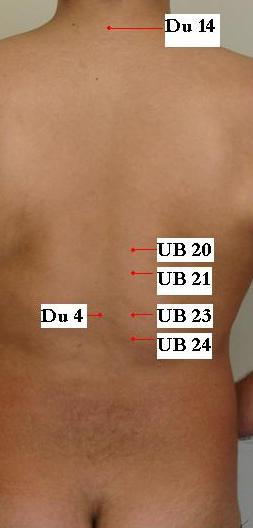
The following acupuncture points usually are selected to treat and help the prevention of osteoporosis.
Dazhui Du14 and Ming Men Du4 and also Pi Shu UB20, Wei Shu UB21, Shen Shu UB23, and Qi Hai Shu UB24.
Pic 43-1
See graph below for explanation of picture above: